PART I. THE FIVE-FINGER APPROACH TO CARDIAC DIAGNOSIS
CHAPTER 1. THE CARDIAC HISTORY
Chest Pain or Discomfort
- Coronary Artery Disease (CAD)
- Stable Angina Pectoris, Unstable Angina, and Acute Myocardial Infarction
- Pertinent Past Medical History and/or Risk Factors for CAD
- Chest Pain in Other Cardiovascular Conditions
- Pericarditis
- Aortic Dissection
- Mitral Valve Prolapse
- Left Ventricular Outflow Tract Obstruction (e.g., Valvular Aortic Stenosis, Hypertrophic Cardiomyopathy)
- Pulmonary Hypertension
Shortness of Breath
Fatigue and Weakness
Cough and Hemoptysis
Palpitations
Dizziness, Near-Syncope, and Syncope
Other Symptoms
- Fever, Chills, and Sweats
- Gastrointestinal Symptoms
- Embolic Symptoms
- Intermittent Claudication
- Changes in Weight
CHAPTER 2. THE CARDIAC PHYSICAL EXAM
Cardiac Anatomy and Physiology
- External Anatomy of the Heart and Great Vessels
- Cardiac Chambers and Blood Flow through the Heart
- The Heart Valves
- Structure of the Heart Wall
- Basic Cardiac Function
Inspection
- General Appearance
- Cutaneous Manifestations (Skin Color, Temperature, Texture)
- Voice
- Jugular Venous Pressure (JVP) and Pulse
- Estimating JVP
- Abdominojugular Test
- Abnormalities of the Venous Wave Form
Palpation
-Blood Pressure and Arterial Pulse
- Abnormalities of Blood Pressure
- Abnormalities of Arterial Pulse
-Precordial Movements and Palpation
Auscultation: "The Music of the Heart"
-The Cardiac Cycle
-Proper Use of the Stethoscope
-Dynamic Auscultation
-Heart Sounds: Normal and Abnormal
- First and Second heart sounds (S1 and S2)
- Auscultation of S1 ("Lub")
- Loud S1
- Faint S1
- Variable Intensity of S1
- Auscultation of S2 ("Dub")
- Intensity and Splitting of S2
- Sounds in Systole
- Ejection Sounds and Systolic Clicks
- Sounds in Diastole
- Third and Fourth Heart Sounds (S3 and S4)
- Other Diastolic Sounds
Heart Murmurs: Systolic, Diastolic, and Continuous
- Systolic Murmurs -- Innocent vs Significant ("Guilty")
- Early-mid Systolic (Ejection) Murmurs
-Innocent Murmurs
-Aortic Stenosis
-Pulmonic Stenosis
-Hypertrophic Obstructive Cardiomyopathy
-Atrial Septal Defect - Holosystolic Murmurs
-Mitral Regurgitation
-Tricuspid Regurgitation
-Ventricular Septal Defect - Late Systolic Murmurs
-Mitral Valve Prolapse - Diastolic Murmurs
-Early Diastolic Murmurs
-Aortic Regurgitation
-Pulmonic Regurgitation
-Middiastolic and Presystolic Murmurs
-Mitral Stenosis
-Tricuspid Stenosis - Continuous Murmurs
-Patent Ductus Arteriosus
-Jugular Venous Hum
-Coronary Arteriovenous Fistula
-Pulmonary Arteriovenous Fistula
-Ruptured Sinus of Valsalva Aneurysm - Miscellaneous
-Pericardial Friction Rubs
CHAPTER 3. ELECTROCARDIOGRAM
Basic Electrocardiography
- Cardiac Electrical Activity and the Electrocardiogram (ECG)
- Standard ECG Leads
Approach to ECG Interpretation
- Rate and Rhythm
- The P Wave
- The QRS
- The T Wave
- The U Wave
- The PR Interval
- The ST Segment
- The QT Interval
- QRS Axis
Major ECG Abnormalities: Diagnostic Clues and Clinical Correlations
- Myocardial Ischemia and Infarction
- Cardiac Chamber Enlargement and Hypertrophy
- Miscellaneous Patterns
- Arrhythmias and Conduction Disturbances
CHAPTER 4. CHEST X-RAY
The Cardiovascular Silhouette, Cardiac Chambers and the Aorta
The Pulmonary Vasculature
The Lung Fields
Thoracic Cage Abnormalities
CHAPTER 5. CARDIAC DIAGNOSTIC LABORATORY TESTS
Blood Tests
- Routine Chemistries
- Cardiac Biomarkers
Specialized Non-invasive Tests
- Transthoracic M-Mode and Two Dimensional Color
- Flow Doppler
- Echocardiography
- Transesophageal Echocardiography
- Ambulatory Electrocardiography; Holter Monitoring and Transtelephonic
- ECG/Event Recording
- Signal Averaged Electrocardiography
- Tilt-Table Testing
- Exercise and Pharmacologic Stress Testing, including
- Nuclear and Echocardiographic Imaging
- Radionuclide Studies
- Electron Beam Computed Tomography
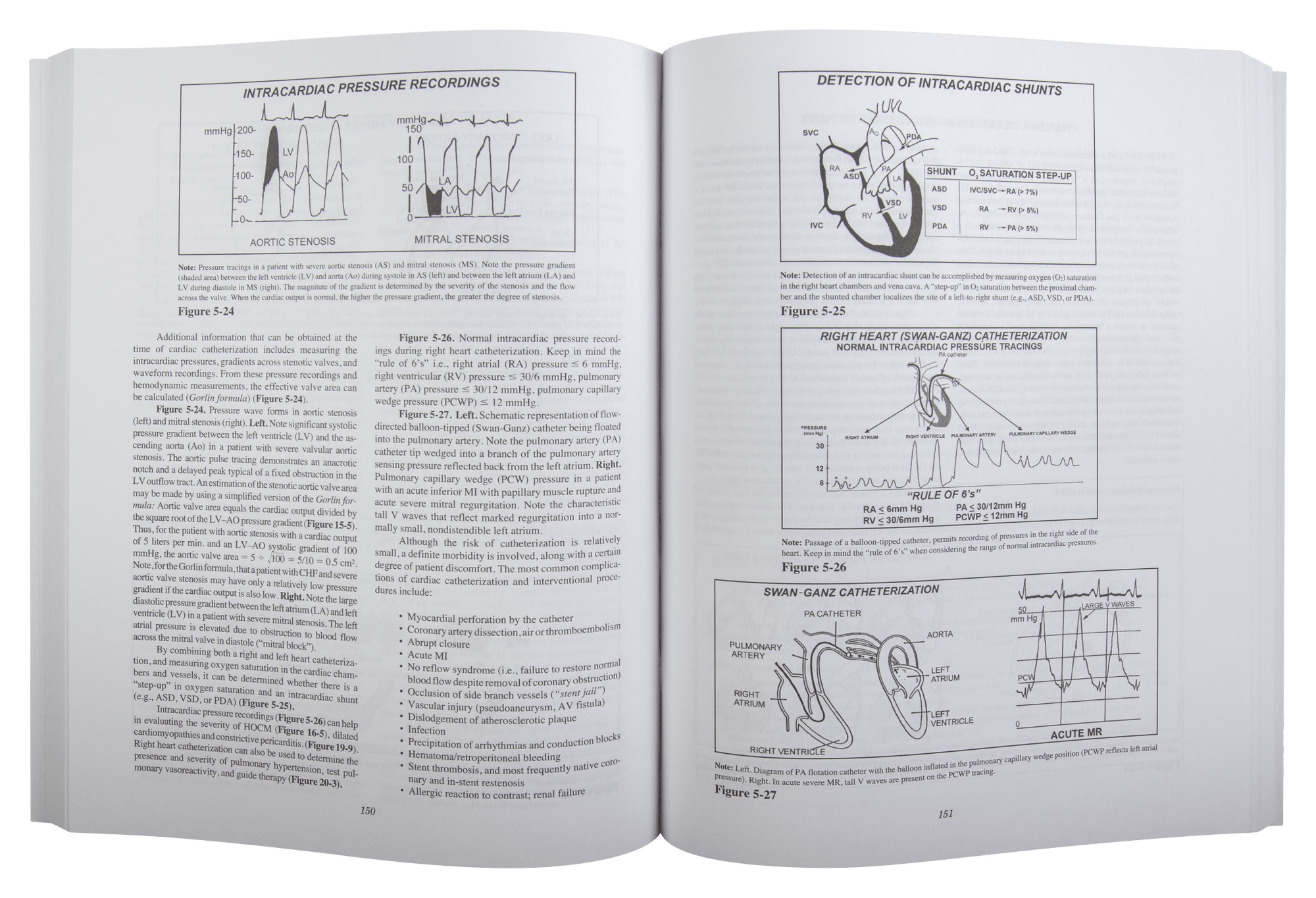
Specialized Invasive Techniques
- Cardiac Catheterization: Coronary Angiography and Left Ventriculography
- Electrophysiologic Studies (EPS)
Summary: Non-invasive and Invasive Test Indications and Applications
PART II. CARDIOVASCULAR THERAPEUTICS
CHAPTER 6. CARDIOVASCULAR THERAPY: AN OVERVIEW
General Considerations and Treatment Goals
Evidence-Based Medicine and Clinical Practice Guidelines
CHAPTER 7. CARDIAC DRUGS
Beta blockers
Calcium Channel Blockers
Nitrates
Angiotensin-Converting Enzyme (ACE) Inhibitors
Angiotensin Receptor Blockers (ARBs)
Angiotensin Receptor Neprilysin Inhibitors (ARNI)
Inotropic Agents
- Digitalis Glycosides
- Sympathomimetic Amines
- Phosphodiesterase Inhibitors
Diuretics
- Thiazides
- Loop Diuretics
- Potassium Sparing Diuretics
Antiplatelet Agents
- Aspirin
- Adenosine Diphosphate (ADP) Receptor Antagonist
- Glycoprotein (GP) IIb/IIIa Receptor Inhibitors
- Thrombin Receptor (PAR-1) Antagonist
Thrombolytics and Anticoagulants
- Thrombolytic Agents
- Unfractionated and Low Molecular Weight Heparin, Direct Thrombin Inhibitors, and Factor Xa Inhibitors
- Vitamin K Antagonists and Novel Oral Anticoagulants (NOACs)
Lipid Controlling Agents
- HMG CoA Reductase Inhibitors (Statins)
- Nicotinic Acid (Niacin)
- Bile Acid Sequestrants (Resins)
- Fibric Acid Derivatives (Fibrates)
- Cholesterol Absorption Inhibitors (e.g., Ezetimibe)
- Proprotein Convertase Subtilisin-Kexin type 9 (PKSK9) Inhibitors
Antiarrhythmic Agents
-Class I Agents
-Class II Agents
-Class III Agents
-Class IV Agents
-Other Agents (e.g., Digitalis, Adenosine)
CHAPTER 8. CARDIAC NONPHARMACOLOGIC AND INTERVENTIONAL TECHNIQUES
- Percutaneous Coronary Intervention (PCI): Percutaneous Transluminal Coronary
Angioplasty (PTCA) and Stenting - Percutaneous Balloon Valvuloplasty, Valve Replacement and/or repair
- Catheter Ablation
- Electrical Cardioversion and Defibrillation
CHAPTER 9. CARDIAC DEVICE THERAPY
- Cardiac Pacemakers
- Implantable Cardioverter Defibrillator
CHAPTER 10. CARDIAC SURGERY
- Coronary Artery Bypass Grafting
- Valvular Repair and/or Replacement
- Cardiac Transplantation
PART III. PUTTING IT ALL TOGETHER
CHAPTER 11. APPROACH TO THE PATIENT WITH CORONARY ARTERY DISEASE
Angina Pectoris
- Clinical Recognition of Stable Angina Pectoris
- Clinical Recognition of Unstable Angina
- Management of Stable Angina Pectoris
- Management of Unstable Angina
Acute Myocardial Infarction (MI)
- Clinical Recognition of Acute MI
- Management of Acute MI
- Complications of Acute MI
- Electrical Complications of Acute MI
- Ventricular Arrhythmias
- Supraventricular Arrhythmias
- Bradyarrhythmias and Conduction Disturbances
- Mechanical Complications of Acute MI
- Left Ventricular (LV) Systolic Dysfunction
- Acute Ventricular Septal Defect and Papillary Muscle
- Rupture
- Right Ventricular Infarction
- Left Ventricular Aneurysm
- LV Free Wall Rupture and Pseudoaneurysm
- Pericarditis
- Secondary Prevention: Pharmacologic Therapy, Risk
- Factor Modification and
Cardiac Rehabilitation
CHAPTER 12. APPROACH TO THE PATIENT WITH HEART FAILURE
- Etiology and Pathophysiology
- Left Ventricular Systolic Dysfunction
- Dilated Cardiomyopathy
- Left Ventricular Diastolic Dysfunction
- Treatment of Chronic Heart Failure
- Treatment of Acute Pulmonary Edema
CHAPTER 13. APPROACH TO THE PATIENT WITH SYSTEMIC ARTERIAL HYERTENSION
- Primary and Secondary Forms of Hypertension
- Clinical Manifestations of Hypertension
- Therapy of Hypertension
CHAPTER 14. APPROACH TO THE PATIENT WITH DYSLIPIDEMIA
- Pathogenesis of Atherosclerosis
- Therapeutic Considerations
CHAPTER 15. APPROACH TO THE PATIENT WITH VALVULAR HEART DISEASE
Aortic Stenosis (AS)
- Clinical Recognition of AS
- Management of AS
Aortic Regurgitation (AR)
- Chronic AR
- Clinical Recognition of Chronic AR
- Acute AR
- Clinical Recognition of Acute AR
- Management of Chronic and Acute AR
Mitral Regurgitation (MR)
- Chronic MR
- Clinical Recognition of Chronic MR
- Management of Chronic MR
- Acute MR
- Clinical Recognition and Management of Acute MR
Mitral Valve Prolapse (MVP)
- Clinical Recognition of MVP
- Management of MVP
Rheumatic Mitral Stenosis (MS)
- Clinical Recognition of Rheumatic MS
- Management of Rheumatic MS
Tricuspid Regurgitation (TR)
- Clinical Recognition of TR
- Management of TR
CHAPTER 16. APPROACH TO THE PATIENT WITH HYPERTROPHIC CARDIOMYOPATHY
- Clinical Recognition of Hypertrophic Obstructive - Cardiomyopathy (HOCM)
- Treatment Options for HOCM
- Risk of Sudden Death
CHAPTER 17. APPROACH TO THE PATIENT WITH INFECTIVE ENDOCARDITIS
- Etiology and Risk Factors
- Clinical Presentation of Infective Endocarditis
- Therapy of Infective Endocarditis
CHAPTER 18. APPROACH TO THE PATIENT WITH AORTIC DISSECTION
- Classification and Pathogenesis
- Clinical Manifestations of Aortic Dissection
- Medical and Surgical Considerations in Aortic Dissection
CHAPTER 19. APPROACH TO THE PATIENT WITH PERICARDIAL DISEASE
- Acute Pericarditis
- Cardiac Tamponade
- Constrictive Pericarditis
CHAPTER 20. APPROACH TO THE PATIENT WITH PULMONARY HYPERTENSION
- Pathophysiologic Mechanisms
- Clinical Recognition of Primary Pulmonary Hypertension
- Management of Pulmonary Hypertension
CHAPTER 21. APPROACH TO THE PATIENT WITH A HEART MURMUR
- Evaluation of a Heart Murmur: An Integrated Approach
- When to Order a Doppler-Echo
- Clues from the Cardiac Clinical Exam
CHAPTER 22. APPROACH TO THE PATIENT WITH CARDIAC ARRHYTHMIAS AND CONDUCTION DISTURBANCES
- General Considerations
- Atrial Fibrillation
- Supraventricular Tachycardias
- Ventricular Tachycardia
- Bradyarrhythmias and Conduction Abnormalities
CHAPTER 23. APPROACH TO THE PATIENT WITH ADULT CONGENITAL HEART DISEASE
- Bicuspid Aortic Valve
- Pulmonic Valve Stenosis
- Atrial Septal Defect
- Ventricular Septal Defect
- Coarctation of the Aorta
- Patent Ductus Arteriosus
- Marfan's Syndrome
CHAPTER 24. APPROACH TO THE PATIENT WITH HEART DISEASE UNDERGOING NONCARDIAC SURGERY
Preoperative Assessment of Risk
- Clinical Predictors of Risk
- Surgery Specific Markers of Risk
Perioperative Evaluation and Management
CHAPTER 25. APPROACH TO THE PATIENT WITH NEOPLASTIC HEART DISEASE
Primary Tumors of the Heart
- Atrial Myxoma
- Angiosarcoma
Secondary Tumors of the Heart and the Effects of Treatment
Carcinoid Syndrome
CHAPTER 26. APPROACH TO THE PATIENT WITH "FALSE" HEART DISEASE
Pitfalls in the Clinical Recognition and Management of Heart Disease
Misleading Clues in the Clinical Cardiovascular Evaluation
- Misinterpretation of Symptoms and Signs
- Misinterpretation of ECG, CXR, and Diagnostic Laboratory Data
The Athlete's Heart
Iatrogenic Heart Disease
CHAPTER 27. APPROACH TO THE PATIENT WITH AN ACUTE CARDIAC EMERGENCY
- General Considerations
- Universal Approach to Adult Emergency Cardiac Care
- Ventricular Fibrillation/Pulseless Ventricular -Tachycardia
- Pulseless Electrical Activity
- Asystole
- Bradycardia
- Tachycardia
- Shock
Selected Reading
Index